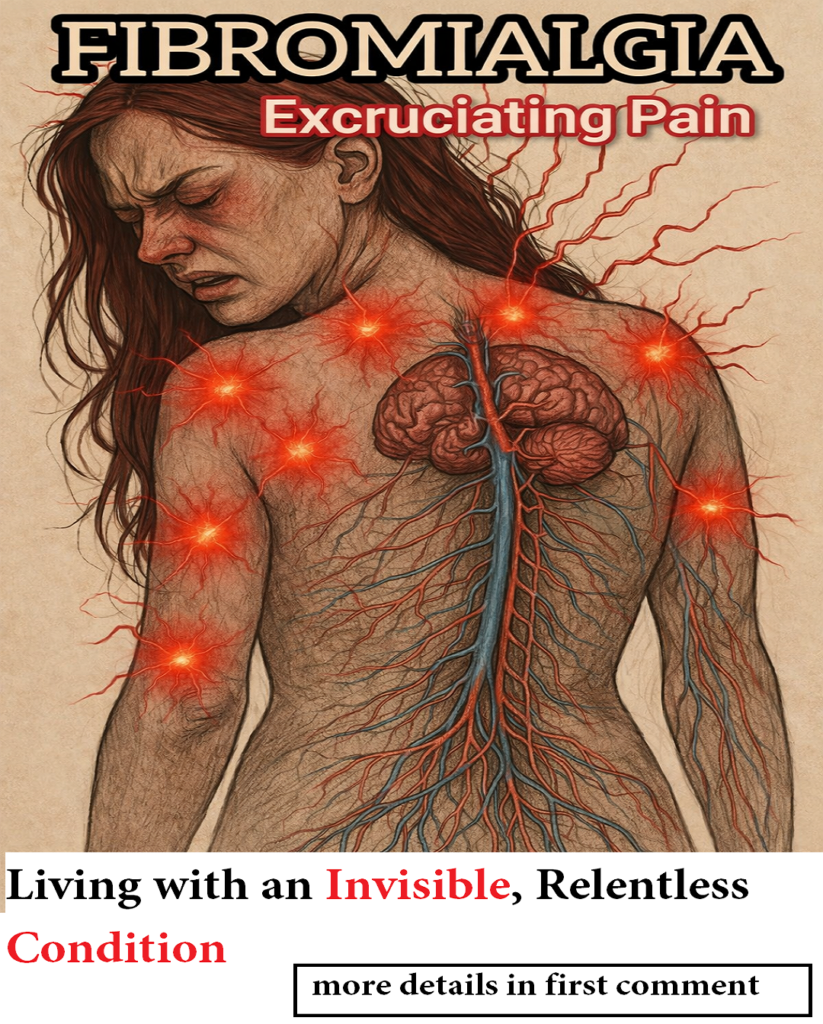
Chronic pain conditions are often misunderstood, especially when the suffering cannot be seen. Fibromyalgia is one of the most complex and invisible illnesses, affecting millions worldwide. When combined with trochanteric bursitis — a common cause of hip pain — the burden becomes even heavier. Together, these conditions create a cycle of persistent discomfort, fatigue, and emotional strain that impacts daily life in profound ways.
This article explores fibromyalgia, trochanteric bursitis, their connection, symptoms, causes, and effective ways to manage this challenging combination.
What Is Fibromyalgia?
Fibromyalgia is a chronic pain disorder characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive difficulties. Unlike injuries or inflammatory diseases, fibromyalgia often leaves no visible signs, making it difficult for others to understand the severity of the condition.
People living with fibromyalgia often describe the pain as deep, constant, and overwhelming — as if it comes from within the body rather than from an external injury. The pain can affect muscles, joints, and nerves simultaneously, creating sensations such as burning, aching, stabbing, or pressure.
Common Symptoms of Fibromyalgia
-
Widespread chronic pain
-
Extreme fatigue and low energy
-
Sleep disturbances or non-restorative sleep
-
Brain fog (memory and concentration problems)
-
Sensitivity to light, sound, touch, and temperature
-
Headaches and migraines
-
Muscle stiffness and weakness
-
Mood disturbances, anxiety, or depression
One of the most distressing aspects of fibromyalgia is its invisibility. Outwardly, a person may appear healthy, yet internally they are battling constant pain and exhaustion. This disconnect often leads to misunderstanding, frustration, and emotional fatigue.
The Invisible Burden of Chronic Pain
Fibromyalgia does not bruise the skin or appear clearly on routine medical tests, but its impact is very real. The body remains in a state of heightened sensitivity, where the nervous system amplifies pain signals. Even mild physical strain or emotional stress can trigger intense discomfort.
This persistent pain drains energy, disrupts focus, and interferes with everyday tasks. Activities that seem simple — walking, climbing stairs, or even concentrating — can become exhausting challenges. Over time, the combination of physical pain and emotional strain can significantly reduce quality of life.
Living with fibromyalgia requires resilience, patience, and strength. Recognition and understanding from others play a crucial role in helping individuals cope with this invisible illness.
What Is Trochanteric Bursitis?
Trochanteric bursitis is a common cause of outer hip pain. It occurs when the trochanteric bursa — a small fluid-filled sac located on the outer side of the hip — becomes inflamed.
The bursa acts as a cushion, reducing friction between muscles, tendons, and the femur bone. When irritated or inflamed, it causes localized pain and tenderness around the hip.
Common Symptoms of Trochanteric Bursitis
-
Sharp or aching pain on the outer hip
-
Pain that worsens when walking, climbing stairs, or standing
-
Discomfort when lying on the affected side
-
Hip tenderness when touched
-
Pain radiating to thigh or buttock
-
Stiffness and reduced hip movement
Trochanteric bursitis may result from repetitive movement, injury, poor posture, muscle weakness, or mechanical overload.
The Link Between Fibromyalgia and Trochanteric Bursitis
Fibromyalgia and trochanteric bursitis often coexist, and their interaction can intensify pain and discomfort. While bursitis causes localized inflammation, fibromyalgia affects how the brain and nervous system process pain signals.
In fibromyalgia, the nervous system is highly sensitive, meaning even mild inflammation can feel severe. This phenomenon is known as central sensitization, where the brain amplifies pain perception.
When trochanteric bursitis occurs alongside fibromyalgia:
-
Pain becomes more widespread and persistent
-
Recovery may take longer
-
Sleep disturbances worsen
-
Fatigue increases
-
Movement becomes more difficult
The coexistence of these conditions demonstrates that chronic pain often has multiple contributing factors, including inflammation, mechanical strain, and nervous system dysfunction.
Why Hip Pain Feels Worse in Fibromyalgia
In individuals with fibromyalgia, hip pain from bursitis can feel stronger and more widespread than expected. Several factors contribute to this:
1. Central Nervous System Sensitization
The brain becomes more responsive to pain signals, amplifying even minor inflammation.
2. Muscle Stiffness and Weakness
Fibromyalgia often causes muscle tightness and weakness, placing additional strain on the hip joint and surrounding tissues.
3. Altered Gait and Movement
Pain and fatigue can change walking patterns, increasing pressure on the hip and worsening bursitis.
4. Sleep Disturbances
Poor sleep reduces the body’s ability to repair tissues, prolonging inflammation and pain.
Pain Radiation and Misdiagnosis
Pain from trochanteric bursitis often spreads to nearby areas, including:
-
Outer thigh
-
Buttocks
-
Lower back
This spreading pain can sometimes resemble sciatica, leading to misdiagnosis. However, unlike sciatica, bursitis pain typically worsens when lying on the affected side or pressing the hip.
Accurate diagnosis is essential to ensure proper treatment and pain management.
Emotional and Psychological Impact
Chronic pain conditions like fibromyalgia do not only affect the body — they also influence emotional well-being.
Many individuals experience:
-
Frustration due to lack of visible symptoms
-
Emotional exhaustion from constant pain
-
Anxiety about future health
-
Depression caused by reduced mobility and energy
-
Stress from needing to explain or justify their pain
Understanding and empathy from family, friends, and healthcare providers play a vital role in improving emotional health.
Diagnosis and Medical Evaluation
There is no single test to diagnose fibromyalgia. Doctors usually rely on:
-
Medical history
-
Pain duration and distribution
-
Symptom patterns
-
Physical examination
Trochanteric bursitis may be diagnosed through:
-
Physical examination
-
Imaging tests (ultrasound or MRI if needed)
-
Assessment of hip tenderness and movement
Proper diagnosis helps create an effective treatment plan tailored to the patient’s needs.
Treatment and Pain Management
Managing fibromyalgia and trochanteric bursitis together requires a multidimensional approach.
1. Physical Therapy
Strengthening hip and core muscles helps reduce strain on the bursa and improves mobility.
2. Gentle Exercise
Low-impact activities such as walking, swimming, or stretching improve circulation, reduce stiffness, and enhance overall well-being.
3. Pain Relief Strategies
Doctors may recommend medications, anti-inflammatory treatments, or localized therapies to reduce pain and inflammation.
4. Sleep Improvement
Good sleep hygiene supports tissue repair and reduces fatigue.
5. Stress Management
Relaxation techniques such as meditation, breathing exercises, or mindfulness help calm the nervous system.
6. Lifestyle Adjustments
Avoiding prolonged pressure on the hip, maintaining good posture, and pacing daily activities can prevent flare-ups.
Living with Invisible Pain
Living with fibromyalgia and trochanteric bursitis requires daily strength. The pain may not be visible, but its impact is real and significant.
People with these conditions often learn to:
-
Respect their body’s limits
-
Balance activity and rest
-
Seek emotional and medical support
-
Adapt their lifestyle for long-term health
Recognition and awareness are essential. Invisible pain deserves understanding, compassion, and proper care.
When to Seek Medical Help
Consult a healthcare professional if:
-
Hip pain persists for weeks
-
Pain interferes with sleep or mobility
-
Symptoms worsen over time
-
Fatigue becomes overwhelming
-
Pain spreads or changes pattern
Early treatment can prevent complications and improve quality of life.
Final Thoughts
Fibromyalgia is pain that crushes from within, leaving no visible marks yet deeply affecting body and mind. Trochanteric bursitis adds another layer of discomfort through localized hip inflammation. Together, they highlight the complex nature of chronic pain — involving the nervous system, muscles, and emotional resilience.
Although invisible, this pain is real. Those living with fibromyalgia and bursitis demonstrate remarkable strength every day. Understanding, proper care, and compassionate support can make a meaningful difference in managing this challenging journey.
Invisible pain still deserves recognition, respect, and serious attention — because healing begins with understanding.